|
Journal of Urban Design and Mental Health 2017;2:1
|
Architecture, the urban environment and severe psychosis: Aetiology
Jan Golembiewski BFA, BArch MArch PhD, Regd. Architect
Psychological Design and Schizophrenia Research Institute, Australia
Psychological Design and Schizophrenia Research Institute, Australia
Abstract
The finding that schizophrenia and other severe psychoses are largely urban phenomena raises questions about why this is the case and how the physical environment affects the brain. This article outlines the background for the Ecological Hypothesis for Schizophrenia, proposing that any environment makes demands on people, and that these can be naturally inhibited, especially if the nature of the demands are unsavoury or unwanted. But a person’s inhibition reflex decreases in the face of a continual onslaught of demands to the point where the person just can’t cope; the result is a series of unwanted and often undesirable reactions to the demands of the phenomenological environment.
Both social and physical environments trigger demands, but the latter is usually more insidious. This is especially true in the urban environment because every part of it is deliberately designed to assert meanings and messages. These demands trigger action and thought on a latent level of awareness, and become more potent as an inability to ‘cope’ sets in. This is because dopamine, the neurotransmitter that’s thought to moderate the saliency of phenomena is also what gives perceptions more compulsive power. As phenomenological experience spirals further out of control with on-going environmental stimulation, so too will dopamine. The automatic behaviours that the environment triggers are the major symptoms that we recognise as psychosis.
This article is Part 1 of a pair of articles describing the complex relationship between severe psychosis and the environment.
The finding that schizophrenia and other severe psychoses are largely urban phenomena raises questions about why this is the case and how the physical environment affects the brain. This article outlines the background for the Ecological Hypothesis for Schizophrenia, proposing that any environment makes demands on people, and that these can be naturally inhibited, especially if the nature of the demands are unsavoury or unwanted. But a person’s inhibition reflex decreases in the face of a continual onslaught of demands to the point where the person just can’t cope; the result is a series of unwanted and often undesirable reactions to the demands of the phenomenological environment.
Both social and physical environments trigger demands, but the latter is usually more insidious. This is especially true in the urban environment because every part of it is deliberately designed to assert meanings and messages. These demands trigger action and thought on a latent level of awareness, and become more potent as an inability to ‘cope’ sets in. This is because dopamine, the neurotransmitter that’s thought to moderate the saliency of phenomena is also what gives perceptions more compulsive power. As phenomenological experience spirals further out of control with on-going environmental stimulation, so too will dopamine. The automatic behaviours that the environment triggers are the major symptoms that we recognise as psychosis.
This article is Part 1 of a pair of articles describing the complex relationship between severe psychosis and the environment.
| Full text PDF: Architecture, the urban environment, and severe psychosis |
A case for the Ecological Hypothesis for Schizophrenia
There has been a growing interest in the consistent finding that the urban environment appears to be the locus of the epidemic of schizophrenia and other severe psychotic conditions (Kelly et al., 2010; van Os, 2010), but of the dozens of studies and reviews that support this observation, most make frustrating reading for concerned designers because very few address the issues that city builders face in praxis. These texts leave us wondering what built-environment professionals (policy-developers, planners, urban designers, developers, architects and other designers) can do alleviate the problem and perhaps even prevent mental illness. But before we head for conclusions, it is critical to understand the Ecological Hypothesis for Schizophrenia, and where it stands alongside current epidemiological thinking in this space. As we shall see shortly, the theory is tenable but even so, any relationships that draw together the built environment and mental illness will be regarded with suspicion because the idea contradicts an engrained axiom of modern medicine: the assumption that the brain is a cognition machine and mental illness is a fault in the machinery, not the input (the phenomenological environment) (Golembiewski, 2016).
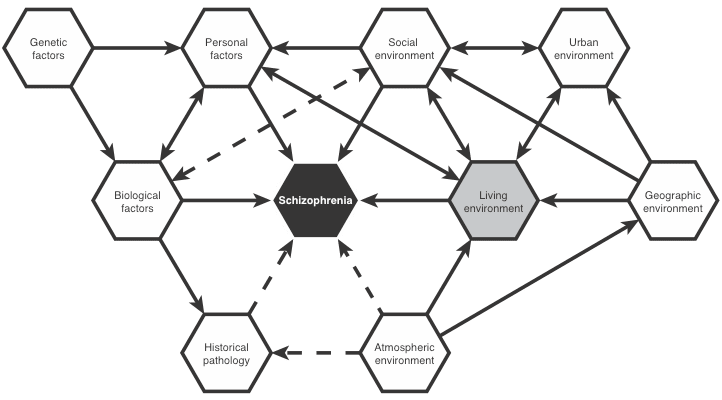
As Kelly and O'Callaghan report, the epidemiology of severe psychotic illness is strikingly prevalent in urban areas – to the extent that this may be the single largest and most robust finding about the spectrum of psychotic conditions (Kelly et al., 2010) There are a few hypotheses that attempt to grapple with this data, but none have especially robust correlations between the proposed active agents and the outcomes – that is the symptomatology of psychosis. For this reason, most scientists focus on either broad, sweeping conditions like ‘social failure,’ (Selten and Cantor-Graae, 2007) or what are called ‘multi-factor hypotheses’ (Figure 1). These follow the tradition of the original (and well-worn) hypothesis for the epidemiology of ‘insanity’ (1) tested in Chicago during the prohibition period of the 1930s. Only once they had failed to identify the ‘smoking gun’ of the insanity epidemic, using Snow’s mapping method of 1854, Faris and Dunham (1939) identified what they assumed to be ‘breeder’ factors (race, migration status, poverty, the availability of illicit alcohol and access to sunlight), which they pitted against what seemed like the only other available option: the ‘drift effect,’ where people with a high risk of insanity are propelled to the city centres by downward social mobility. Many decades later studies have found that the geographical drift effect is only small (Zammit et al., 2010; Torrey and Bowler, 1990), and that it is an upbringing in a socially deprived area of any big metropolis that repeatedly appears in meta-analyses as the leading predictor of schizophrenia and other severe psychoses (Kirkbride et al., 2012).
To understand this data (generations later), studies are still identifying very similar multifactor risks to those identified by Faris and Dunham. A great deal of thought has also gone into understanding how these small effect risk factors can possibly compound to cause the illness (Freeman and Alpert, 1986).
At times, multi-factor hypotheses yield compelling correlation data. However, data does not prove an aetiological pathway because it is a fallacy to take a correlation as the cause. (This is where evidence is taken as proof, although no reasonable relationship can be established.) Errors of this kind are relatively common in schizophrenia research: absurd postulations abound, but fortunately academic rigour usually prevails and few are published. Of those that somehow slipped past the editor, there is an entertaining heeled-shoe hypothesis (Flensmark, 2004), a water-intoxication hypothesis (de Leon et al., 1994) and a body-shape hypothesis (Kellett, 1973). The best way to protect against fallacious associations is to replicate the data in different circumstances, where the chance of repeating a coincidence is lower than that of winning a lottery, unless the correlation has either a genuine causal effect or because of repeated interference due to an unnoticed confounding variable.
In this regard, the incidence of severe psychosis has independently, consistently and evenly been shown to have a dose-dependent, raised incidence of schizophrenia in urban centres throughout the world once known confounders like drift are controlled (Tost et al., 2015; Morgan, 2010; van Os et al., 2010). The Ecological Hypothesis for Schizophrenia (that the urban environment has a causal relationship with severe psychosis) is quite robust. In fact, when tested against a null hypothesis, and when controlled for other known factors (such as race, genes and cannabis usage), meta-analyses find that the urban environment as place of birth increases the odds of developing schizophrenia in 28-34.3% of all cases (Kelly et al., 2010). There is also correlating data showing altered brain morphology for similar urban cohorts (Haddad et al., 2014; Lederbogen et al., 2013, Lederbogen et al., 2011). The same cannot be said for many of the theories forwarded to explain this phenomena (Golembiewski, 2013), including more highly regarded theories such as the Social Failure Hypothesis (Selten et al., 2007) or the Developmental Vitamin D Deficiency Hypothesis (Eyles et al., 2009), although the latter at least has compelling support from neurological research linking the theory to plausible biological pathways (Cui et al., 2009).
Figure 1
There has been a growing interest in the consistent finding that the urban environment appears to be the locus of the epidemic of schizophrenia and other severe psychotic conditions (Kelly et al., 2010; van Os, 2010), but of the dozens of studies and reviews that support this observation, most make frustrating reading for concerned designers because very few address the issues that city builders face in praxis. These texts leave us wondering what built-environment professionals (policy-developers, planners, urban designers, developers, architects and other designers) can do alleviate the problem and perhaps even prevent mental illness. But before we head for conclusions, it is critical to understand the Ecological Hypothesis for Schizophrenia, and where it stands alongside current epidemiological thinking in this space. As we shall see shortly, the theory is tenable but even so, any relationships that draw together the built environment and mental illness will be regarded with suspicion because the idea contradicts an engrained axiom of modern medicine: the assumption that the brain is a cognition machine and mental illness is a fault in the machinery, not the input (the phenomenological environment) (Golembiewski, 2016).
As Kelly and O'Callaghan report, the epidemiology of severe psychotic illness is strikingly prevalent in urban areas – to the extent that this may be the single largest and most robust finding about the spectrum of psychotic conditions (Kelly et al., 2010) There are a few hypotheses that attempt to grapple with this data, but none have especially robust correlations between the proposed active agents and the outcomes – that is the symptomatology of psychosis. For this reason, most scientists focus on either broad, sweeping conditions like ‘social failure,’ (Selten and Cantor-Graae, 2007) or what are called ‘multi-factor hypotheses’ (Figure 1). These follow the tradition of the original (and well-worn) hypothesis for the epidemiology of ‘insanity’ (1) tested in Chicago during the prohibition period of the 1930s. Only once they had failed to identify the ‘smoking gun’ of the insanity epidemic, using Snow’s mapping method of 1854, Faris and Dunham (1939) identified what they assumed to be ‘breeder’ factors (race, migration status, poverty, the availability of illicit alcohol and access to sunlight), which they pitted against what seemed like the only other available option: the ‘drift effect,’ where people with a high risk of insanity are propelled to the city centres by downward social mobility. Many decades later studies have found that the geographical drift effect is only small (Zammit et al., 2010; Torrey and Bowler, 1990), and that it is an upbringing in a socially deprived area of any big metropolis that repeatedly appears in meta-analyses as the leading predictor of schizophrenia and other severe psychoses (Kirkbride et al., 2012).
To understand this data (generations later), studies are still identifying very similar multifactor risks to those identified by Faris and Dunham. A great deal of thought has also gone into understanding how these small effect risk factors can possibly compound to cause the illness (Freeman and Alpert, 1986).
At times, multi-factor hypotheses yield compelling correlation data. However, data does not prove an aetiological pathway because it is a fallacy to take a correlation as the cause. (This is where evidence is taken as proof, although no reasonable relationship can be established.) Errors of this kind are relatively common in schizophrenia research: absurd postulations abound, but fortunately academic rigour usually prevails and few are published. Of those that somehow slipped past the editor, there is an entertaining heeled-shoe hypothesis (Flensmark, 2004), a water-intoxication hypothesis (de Leon et al., 1994) and a body-shape hypothesis (Kellett, 1973). The best way to protect against fallacious associations is to replicate the data in different circumstances, where the chance of repeating a coincidence is lower than that of winning a lottery, unless the correlation has either a genuine causal effect or because of repeated interference due to an unnoticed confounding variable.
In this regard, the incidence of severe psychosis has independently, consistently and evenly been shown to have a dose-dependent, raised incidence of schizophrenia in urban centres throughout the world once known confounders like drift are controlled (Tost et al., 2015; Morgan, 2010; van Os et al., 2010). The Ecological Hypothesis for Schizophrenia (that the urban environment has a causal relationship with severe psychosis) is quite robust. In fact, when tested against a null hypothesis, and when controlled for other known factors (such as race, genes and cannabis usage), meta-analyses find that the urban environment as place of birth increases the odds of developing schizophrenia in 28-34.3% of all cases (Kelly et al., 2010). There is also correlating data showing altered brain morphology for similar urban cohorts (Haddad et al., 2014; Lederbogen et al., 2013, Lederbogen et al., 2011). The same cannot be said for many of the theories forwarded to explain this phenomena (Golembiewski, 2013), including more highly regarded theories such as the Social Failure Hypothesis (Selten et al., 2007) or the Developmental Vitamin D Deficiency Hypothesis (Eyles et al., 2009), although the latter at least has compelling support from neurological research linking the theory to plausible biological pathways (Cui et al., 2009).
Figure 1
Figure 1. This diagram shows relationships between the commonly studied hypothetical aetiological factors. Of these, the living and work environments (grey) are the nexus of; the social environment, the urban environment, geography, the quality and tenure of housing, availability of sunlight and quality of artificial light, air quality, climatic and somatic comfort, fungal and bacterial growth, presence of pets and vermin or other animals.
The effect the physical environment has on human psychology is continually overlooked as a causal factor even though it has an influence on nearly every other factor that has ever been targeted in the search for the aetiology of severe psychosis so far – the main exception being genetics (and even then, in cities people often cluster by race). The physical environment (especially at an urban scale) lends itself to multi-factor hypotheses. It has a powerful influence on the social milieu for instance – there is perhaps no stronger social segregator than the walls and doors that the built environment is made of. And the built environment also has a profound effect on other possible aetiological factors; the civic, geographical, demographic, personal and other ecological influences like poverty, drug-usage, available sunlight (vitamin D), pollution and even quality of healthcare and education. All can be accommodated within the Ecological Hypothesis for Schizophrenia.
Perhaps this focus on individual factors misses the wood for the trees. The living environment as a whole (home) provides the principal filter for the ecological effects of the urban environment (also taken as a whole). In other words, a nice and secure home provides respite. In addition, the living environment also represents the primary developmental milieu: the environment for on-going discovery and self-development throughout life. The aetiological influence we see in the urban setting may then reflect a long-tern lack of opportunity to relax, recover and take respite; or perhaps a lack of opportunity to learn the lessons needed to withstand life’s pressures outside of home - or both. This simple reading of an extraordinarily complex situation my also explain outlier data – such as cases where a rural lifestyle was not sufficient to allow a child respite and avoid a future breakdown.
The background science
Ecological theories have been proposed before (Zubin and Spring, 1977), but perhaps the main problem people have with the Ecological Hypothesis for Schizophrenia is that we know very little about psychosis (Mujica-Parodi et al., 2000) except that since the 1960s, the most effective way to reduce delusions, hallucinations, violence and other overt symptoms has been by administering dopamine-receptor blocking medications (Ginovart and Kapur, 2010). This means the gold standard for schizophrenia hypotheses is a convincing explanation for this effect, and any attempt to bypass the background science and receive much attention. But while people are slowly coming around to the idea that the mind and body may be connected, a much larger leap is required to accept that the built environment somehow moderates the dopamine pathway within the brain.
In 2003 Shitij Kapur, one of the most prominent researchers of the dopamine system, published ‘the Aberrant Salience Hypothesis,’ which asserts that dopamine mediates a person’s sense of salience (Kapur, 2003). In other words, it reduces the feeling that irrelevant stimuli are important. Since 2003 the theory has been cited more than 1000 times as supporting evidence is gathered, and now it is fair to say the theory has become the most widely held perspective on the function of the dopamine neurotransmitter in psychotic disorders (For example: Haselgrove et al., 2016; Stephan, 2016). Put simply, the mesolimbic dopamine system manages the significance (or salience) of information using the dopamine neurones that run from the source of dopamine in the central region of the brain, through the striatum and limbic area, through the anterior cingulate cortex (ACC) and terminates in the frontal cortex (FC). Each of these areas are responsible for different functions – but essentially the first part provides the low levels of attention that are required for automatic and semi-automatic functions, thoughts and tasks. The ACC and FC extension, on the other hand, provides the engaged-type of ‘declarative’ attention that we need to be genuinely conscious of our actions and thoughts (Rigoli et al., 2016; Golembiewski, 2013). The Aberrant Salience Hypothesis holds that some unknown dysfunction upsets the dopamine system, thereby causing stimuli to appear important when they are not, whilst genuinely important things can be overlooked (Kapur, 2003). The Ecological Hypothesis for Schizophrenia accepts the Aberrant Salience Hypothesis, but goes further to assert that the trigger is not bad wiring in the brain. Instead, the cause is consistent exposure to genuinely salient and negative environmental circumstances (both social and the product of architectural and urban design) whenever these environmental factors fail to provide respite when it is needed.
There is ample evidence that the relationship between the environment and the brain is much stronger than most scientists acknowledge. More than 95% of adult actions and thoughts are not the end result of deliberate cognition and planning, but are precognitive, automatic responses (Baumeister and Sommer, 1997). These are largely triggered by the environment – both social (if other people are around – a rare thing for people with advanced psychosis) and also the physical environment (Bargh and Dijksterhuis, 2001). These reactive actions are not very noticeable because they take place with low levels of awareness and as whole ‘events.’ On a neurological level, these are called event-potentials; a series of interrelated neural actions that commence with an excitatory phase and end when the actions are either inhibited or turn into action, which happens whenever there is any surplus excitation. (Effectively the event potential is a zero-sum game).
Emotional associations play a role here also. When the surplus is positive in nature, actions include positive thoughts, laughter, smiles and other desirable actions. But if the surplus of an action potential is triggered by adverse perceptions, people panic. They will jump, scream and experience other behaviours that strongly resemble psychotic symptoms such as thought insertion, confusion and anger. Obviously, the main difference between healthy and mentally ill responses is where the normative reaction threshold is, relative to the context - if there are genuine reasons to feel paranoid, the desire to flee is understandable (Golembiewski, 2012; Freeman and Freeman, 2008). Where the surplus excitation ends up in the brain determines the type of reaction that takes place, and neuroscientists are working hard to discover which part of the brain triggers exactly which actions (thought, visual imagination, reflexes, muscle-movement planning etc.) (Wilson et al., 2010; Trojano et al., 2000).
Everybody recognises automatic impulses to some degree - the impulse to brake when a dog runs in front of a car, the impulse to jump and scream at a sudden fright, to eat food or drink when it is presented, or even to leap at the edge of a cliff. Some of these impulses are uninhibited (braking, for example), others are fully inhibited (actually leaping off a cliff’s edge, for example) and others are contextually resolved so that our reactions remain appropriate (we eat and drink, at home, but not in the supermarket for example). Interestingly people with poor frontal inhibition due to mental illness, intoxication or biological frontal brain damage have far lower (or even no) ability to inhibit these environmental impulses (Lhermitte et al., 1986). This suggests that the primary action of the frontal lobe of the brain is to inhibit the actions that are triggered by circumstance rather than to plan actions in the way that the traditional cognitive model of neuroscience suggests. The more salient a trigger, the stronger the neural event potential and the greater a person’s inhibition needs to be to prevent an inappropriate reactive action.
This is where the built environment may become psychotoxic. Designers deliberately seek salience, and not only for the greater good. Design purposefully elicits responses; to impress, to spur on commerce, to alter behaviour. Also, design is ubiquitous in the urban environment (in contrast to rural environments). In the city, virtually every piece of litter has design intention; every building, billboard, shop window and flashing light contains instructions and meanings (Golembiewski, 2016). Even social exchanges cannot be meaningfully separated from the designed context. Not only do walls separate one person and another (as mentioned above), but we also literally clad ourselves in design. The more urban our lives are, the more we dress and apply cosmetics with greater regard for impressions, and to signify various meanings than just to keep warm.
With the ubiquity of design, it is easy to imagine the slightest mental breakdown spiralling out of control. Already our actions are more or less entirely determined by others – through the language of design. But imagine the alarm people feel when that reality becomes apparent? When we notice that our actions are not mediated by our own choices nor by our own desires? How is this reality to be reconciled? As it happens, the sensation that we are not in control of our lives, and that there is some kind of malevolent force pulling our strings (paranoia) is the most common symptom of schizophrenia (McGrath et al., 2009). Indeed, a close reading of the symptoms alongside the predicted effect of the urban environment on overwrought people’s ability to cope is remarkably tight, suggesting that the designed environment (as a whole, rather than in parts) may indeed be the primary cause of the modern severe psychosis epidemic. This startling insight leads us to question whether we can use design for good, to prevent mental illness and enable recovery - but that is the material for the next article in the series: Architecture, the Urban Environment and Severe Psychosis. Part 2: Design for recovery.
Conclusion
There is a cogent and growing body of evidence demonstrating that severe psychoses (including schizophrenia) are caused by the repetitive onslaught of emotionally negative, yet demanding phenomenological experience. This is not only in the social environment, but in the physical, designed environment also. Indeed, when psychosis is severe, the social environment is usually depleted and social dysfunction is a standard diagnostic criteria of schizophrenia (American Psychiatric Association, 2013).
The Ecological Hypothesis for Schizophrenia asserts that overt psychotic symptoms can be directly triggered by constant demands of the environment, especially where these demands are emotionally negative in nature and when they trigger the kinds of reactions that take place with low levels of self-awareness. An ecological maelstrom of demands constantly acts on everyone, but it is only when our natural ability to appropriately inhibit the demand/action pathway is limited that we start to suffer symptoms. This typically occurs as a failure to cope with the pressing demands of the urban environment, a failure that spirals out of control. Whereas the demands of the social environment are easily understood (they are communicated with verbal and body language), the demands of the physical environment are far subtler, and are more insidious because we assume they are not real. Additionally, the designed environment is particularly demanding – marketers and other designers test and develop special techniques to increase the perceptual salience of their designs and messages.
The prevalence of psychosis in urban environments is therefore hypothesised to be because there is nowhere else where design is more ubiquitous than in the city, where literally every piece of rubbish carries meaning and potentially triggers action. Outside of the cities, demands (whilst still there) are simply far less ubiquitous and largely emerge from the vagaries of nature, rather than by design, and thus the demands of a rural environment are less pointed, personal and emotionally taxing.
Anti-psychotic, dopamine blocking medications help relieve symptoms by allowing sufferers of psychosis some relief by suppressing the saliency of perceptual stimuli, meaning that perceived meanings, whilst usually still there (Schneider et al., 2011), no longer prove to be so demanding. Dopamine is widely believed to mediate saliency after all.
Recommendations for the design of recovery-oriented environments will follow in the next article in this series in Edition 3: Architecture, the Urban Environment and Severe Psychosis. Part 2: Design for recovery. Until then, please feel free to contact the author to add to this material or for advice about designing for better mental health.
Perhaps this focus on individual factors misses the wood for the trees. The living environment as a whole (home) provides the principal filter for the ecological effects of the urban environment (also taken as a whole). In other words, a nice and secure home provides respite. In addition, the living environment also represents the primary developmental milieu: the environment for on-going discovery and self-development throughout life. The aetiological influence we see in the urban setting may then reflect a long-tern lack of opportunity to relax, recover and take respite; or perhaps a lack of opportunity to learn the lessons needed to withstand life’s pressures outside of home - or both. This simple reading of an extraordinarily complex situation my also explain outlier data – such as cases where a rural lifestyle was not sufficient to allow a child respite and avoid a future breakdown.
The background science
Ecological theories have been proposed before (Zubin and Spring, 1977), but perhaps the main problem people have with the Ecological Hypothesis for Schizophrenia is that we know very little about psychosis (Mujica-Parodi et al., 2000) except that since the 1960s, the most effective way to reduce delusions, hallucinations, violence and other overt symptoms has been by administering dopamine-receptor blocking medications (Ginovart and Kapur, 2010). This means the gold standard for schizophrenia hypotheses is a convincing explanation for this effect, and any attempt to bypass the background science and receive much attention. But while people are slowly coming around to the idea that the mind and body may be connected, a much larger leap is required to accept that the built environment somehow moderates the dopamine pathway within the brain.
In 2003 Shitij Kapur, one of the most prominent researchers of the dopamine system, published ‘the Aberrant Salience Hypothesis,’ which asserts that dopamine mediates a person’s sense of salience (Kapur, 2003). In other words, it reduces the feeling that irrelevant stimuli are important. Since 2003 the theory has been cited more than 1000 times as supporting evidence is gathered, and now it is fair to say the theory has become the most widely held perspective on the function of the dopamine neurotransmitter in psychotic disorders (For example: Haselgrove et al., 2016; Stephan, 2016). Put simply, the mesolimbic dopamine system manages the significance (or salience) of information using the dopamine neurones that run from the source of dopamine in the central region of the brain, through the striatum and limbic area, through the anterior cingulate cortex (ACC) and terminates in the frontal cortex (FC). Each of these areas are responsible for different functions – but essentially the first part provides the low levels of attention that are required for automatic and semi-automatic functions, thoughts and tasks. The ACC and FC extension, on the other hand, provides the engaged-type of ‘declarative’ attention that we need to be genuinely conscious of our actions and thoughts (Rigoli et al., 2016; Golembiewski, 2013). The Aberrant Salience Hypothesis holds that some unknown dysfunction upsets the dopamine system, thereby causing stimuli to appear important when they are not, whilst genuinely important things can be overlooked (Kapur, 2003). The Ecological Hypothesis for Schizophrenia accepts the Aberrant Salience Hypothesis, but goes further to assert that the trigger is not bad wiring in the brain. Instead, the cause is consistent exposure to genuinely salient and negative environmental circumstances (both social and the product of architectural and urban design) whenever these environmental factors fail to provide respite when it is needed.
There is ample evidence that the relationship between the environment and the brain is much stronger than most scientists acknowledge. More than 95% of adult actions and thoughts are not the end result of deliberate cognition and planning, but are precognitive, automatic responses (Baumeister and Sommer, 1997). These are largely triggered by the environment – both social (if other people are around – a rare thing for people with advanced psychosis) and also the physical environment (Bargh and Dijksterhuis, 2001). These reactive actions are not very noticeable because they take place with low levels of awareness and as whole ‘events.’ On a neurological level, these are called event-potentials; a series of interrelated neural actions that commence with an excitatory phase and end when the actions are either inhibited or turn into action, which happens whenever there is any surplus excitation. (Effectively the event potential is a zero-sum game).
Emotional associations play a role here also. When the surplus is positive in nature, actions include positive thoughts, laughter, smiles and other desirable actions. But if the surplus of an action potential is triggered by adverse perceptions, people panic. They will jump, scream and experience other behaviours that strongly resemble psychotic symptoms such as thought insertion, confusion and anger. Obviously, the main difference between healthy and mentally ill responses is where the normative reaction threshold is, relative to the context - if there are genuine reasons to feel paranoid, the desire to flee is understandable (Golembiewski, 2012; Freeman and Freeman, 2008). Where the surplus excitation ends up in the brain determines the type of reaction that takes place, and neuroscientists are working hard to discover which part of the brain triggers exactly which actions (thought, visual imagination, reflexes, muscle-movement planning etc.) (Wilson et al., 2010; Trojano et al., 2000).
Everybody recognises automatic impulses to some degree - the impulse to brake when a dog runs in front of a car, the impulse to jump and scream at a sudden fright, to eat food or drink when it is presented, or even to leap at the edge of a cliff. Some of these impulses are uninhibited (braking, for example), others are fully inhibited (actually leaping off a cliff’s edge, for example) and others are contextually resolved so that our reactions remain appropriate (we eat and drink, at home, but not in the supermarket for example). Interestingly people with poor frontal inhibition due to mental illness, intoxication or biological frontal brain damage have far lower (or even no) ability to inhibit these environmental impulses (Lhermitte et al., 1986). This suggests that the primary action of the frontal lobe of the brain is to inhibit the actions that are triggered by circumstance rather than to plan actions in the way that the traditional cognitive model of neuroscience suggests. The more salient a trigger, the stronger the neural event potential and the greater a person’s inhibition needs to be to prevent an inappropriate reactive action.
This is where the built environment may become psychotoxic. Designers deliberately seek salience, and not only for the greater good. Design purposefully elicits responses; to impress, to spur on commerce, to alter behaviour. Also, design is ubiquitous in the urban environment (in contrast to rural environments). In the city, virtually every piece of litter has design intention; every building, billboard, shop window and flashing light contains instructions and meanings (Golembiewski, 2016). Even social exchanges cannot be meaningfully separated from the designed context. Not only do walls separate one person and another (as mentioned above), but we also literally clad ourselves in design. The more urban our lives are, the more we dress and apply cosmetics with greater regard for impressions, and to signify various meanings than just to keep warm.
With the ubiquity of design, it is easy to imagine the slightest mental breakdown spiralling out of control. Already our actions are more or less entirely determined by others – through the language of design. But imagine the alarm people feel when that reality becomes apparent? When we notice that our actions are not mediated by our own choices nor by our own desires? How is this reality to be reconciled? As it happens, the sensation that we are not in control of our lives, and that there is some kind of malevolent force pulling our strings (paranoia) is the most common symptom of schizophrenia (McGrath et al., 2009). Indeed, a close reading of the symptoms alongside the predicted effect of the urban environment on overwrought people’s ability to cope is remarkably tight, suggesting that the designed environment (as a whole, rather than in parts) may indeed be the primary cause of the modern severe psychosis epidemic. This startling insight leads us to question whether we can use design for good, to prevent mental illness and enable recovery - but that is the material for the next article in the series: Architecture, the Urban Environment and Severe Psychosis. Part 2: Design for recovery.
Conclusion
There is a cogent and growing body of evidence demonstrating that severe psychoses (including schizophrenia) are caused by the repetitive onslaught of emotionally negative, yet demanding phenomenological experience. This is not only in the social environment, but in the physical, designed environment also. Indeed, when psychosis is severe, the social environment is usually depleted and social dysfunction is a standard diagnostic criteria of schizophrenia (American Psychiatric Association, 2013).
The Ecological Hypothesis for Schizophrenia asserts that overt psychotic symptoms can be directly triggered by constant demands of the environment, especially where these demands are emotionally negative in nature and when they trigger the kinds of reactions that take place with low levels of self-awareness. An ecological maelstrom of demands constantly acts on everyone, but it is only when our natural ability to appropriately inhibit the demand/action pathway is limited that we start to suffer symptoms. This typically occurs as a failure to cope with the pressing demands of the urban environment, a failure that spirals out of control. Whereas the demands of the social environment are easily understood (they are communicated with verbal and body language), the demands of the physical environment are far subtler, and are more insidious because we assume they are not real. Additionally, the designed environment is particularly demanding – marketers and other designers test and develop special techniques to increase the perceptual salience of their designs and messages.
The prevalence of psychosis in urban environments is therefore hypothesised to be because there is nowhere else where design is more ubiquitous than in the city, where literally every piece of rubbish carries meaning and potentially triggers action. Outside of the cities, demands (whilst still there) are simply far less ubiquitous and largely emerge from the vagaries of nature, rather than by design, and thus the demands of a rural environment are less pointed, personal and emotionally taxing.
Anti-psychotic, dopamine blocking medications help relieve symptoms by allowing sufferers of psychosis some relief by suppressing the saliency of perceptual stimuli, meaning that perceived meanings, whilst usually still there (Schneider et al., 2011), no longer prove to be so demanding. Dopamine is widely believed to mediate saliency after all.
Recommendations for the design of recovery-oriented environments will follow in the next article in this series in Edition 3: Architecture, the Urban Environment and Severe Psychosis. Part 2: Design for recovery. Until then, please feel free to contact the author to add to this material or for advice about designing for better mental health.
Footnotes
(1) The term ‘schizophrenia’ did not come into common usage until the standard diagnostic protocols were published: the ICD-9 (1975) and DSM-III (1980).
(1) The term ‘schizophrenia’ did not come into common usage until the standard diagnostic protocols were published: the ICD-9 (1975) and DSM-III (1980).
References
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. Washington, (5).
Bargh JA, Dijksterhuis A (2001). The perception-behavior expressway: Automatic effects of social perception on social behavior. Advances in experimental social psychology (33), 1-40.
Baumeister RF, Sommer KL (1997). Consciousness, free choice, and automaticity. New Jersey: Lawrence Erlbaum Associates Publishers.
de Leon J, Verghese C, Tracy JI, Josiassen RC, Simpson GM (1994). Polydipsia and water intoxication in psychiatric patients: A review of the epidemiological literature. Biological Psychiatry, 35(6), 408-19.
Cui X, Pelekanos M, Liu PY, Burne TH, McGrath JJ, Eyles DW (2013). The vitamin d receptor in dopamine neurons; its presence in human substantia nigra and its ontogenesis in rat midbrain. Neuroscience, 16(236), 77-87.
Eyles DW, Feron F, Cui X, Kesby JP, Harms LH, Ko P, et al (2009). Developmental vitamin d deficiency causes abnormal brain development. Psychoneuroendocrinology, 34(2), 47-57.
Faris REL, Dunham HW (1939). Mental disorders in urban areas: An ecological study of schizophrenia and other psychoses. Oxford, UK: University of Chicago Press.
Flensmark J (2004). Is there an association between the use of heeled footwear and schizophrenia? Medical Hypotheses, 63(4), 740-7.
Freeman HL, Alpert M (1986). Prevalence of schizophrenia in urban population. The British Journal of Psychiatry, (149), 603-611.
Freeman D, Freeman J (2008). Paranoia the 21st century fear. Oxford, New York: Oxford University Press.
Ginovart N, Kapur S. Dopamine receptors and the treatment of schizophrenia (2010). In: Neve KA, (ed.) The dopamine receptors. New York: Springer, Humana Press, 431-77.
Golembiewski J (2012). All common psychotic symptoms can be explained by the theory of ecological perception. Medical Hypotheses, (78), 7-10.
Golembiewski J (2013). The subcortical confinement hypothesis for schizotypal hallucinations. Curēus, 5(5), 118.
Golembiewski J (2013). Are diverse factors proxies for architectural influences? A case for architecture in the aetiology of schizophrenia. Curēus, 5(3), 106.
Golembiewski J (2016). The designed environment and how it affects brain morphology and mental health. HERD, 9(2), 161-71.
Haddad L, Schafer A, Streit F, Lederbogen F, Grimm O, Wust S, et al (2014). Brain structure correlates of urban upbringing, an environmental risk factor for schizophrenia. Schizophrenia Bulletin.
Haselgrove M, Le Pelley ME, Singh NK, Teow HQ, Morris RW, Green MJ, et al (2016). Disrupted attentional learning in high schizotypy: Evidence of aberrant salience. British Journal of Psychology, 107(4), 601-24.
Kapur S (2003). Psychosis as a state of aberrant salience: A framework linking biology, phenomenology, and pharmacology in schizophrenia. American Journal of Psychiatry, 160(1), 13-23.
Kellett JM (1973). Evolutionary theory for the dichotomy of the functional psychoses. The Lancet. 301(7808), 860-863.
Kelly BD, O'Callaghan E, Waddington JL, Feeney L, Browne S, Scully PJ, et al (2010). Schizophrenia and the city: A review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophrenia Research, 116(1), 75-89.
Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J (2012). Incidence of schizophrenia and other psychoses in england, 1950–2009: A systematic review and meta-analyses. PLOS One, 7(3).
Lederbogen F, Kirsch P, Haddad L, Streit F, Tost H, Schuch P, et al (2011). City living and urban upbringing affect neural social stress processing in humans. Nature, 474(7352), 498-501.
Lederbogen F, Haddad L, Meyer-Lindenberg A (2013). Urban social stress–risk factor for mental disorders. The case of schizophrenia. Environmental Pollution, (183), 2-6.
Lhermitte F (1986). Human autonomy and the frontal lobes. Part II: Patient behavior in complex and social situations: The 'environmental dependency syndrome'. Annals of Neurology, 19(4), 335-43.
Lhermitte F, Pillon B, Serdaru M (1986). Human autonomy and the frontal lobes. Part i: Imitation and utilization behavior: A neuropsychological study of 75 patients. Annals of Neurology, 19(4), 326-34.
McGrath JA, Avramopoulos D, Lasseter VK, Wolyniec PS, Fallin MD, Liang K-Y, et al (2009). Familiality of novel factorial dimensions of schizophrenia. Archives of General Psychiatry, 66(6), 591-600.
Morgan V (2010). Physical environmental risk factors - urban environment. Sydney: Schizophrenia Research Library.
Mujica-Parodi LR, Malaspina D, Sackeim HA (2000). Logical processing, affect, and delusional thought in schizophrenia. Harvard Review of Psychiatry, 8(2), 73-83.
Rigoli F, Friston KJ, Dolan RJ (2016). Neural processes mediating contextual influences on human choice behaviour. Nature Communications, 7(12416).
Schneider SD, Jelinek L, Lincoln TM, Moritz S (2011). What happened to the voices? A fine-grained analysis of how hallucinations and delusions change under psychiatric treatment. Psychiatry Research, 188(1), 13-7.
Selten JP, Cantor-Graae E (2007). Hypothesis: Social defeat is a risk factor for schizophrenia? The British Journal of Psychiatry, 191(51), 9-12.
Stephan KE (2016). Bayesian inference, dysconnectivity and neuromodulation in schizophrenia. Brain, 139:(187), 4-6.
Torrey EF, Bowler A (1990). Geographical distribution of insanity in america: Evidence for an urban factor. Schizophrenia Bulletin, 16(4), 591-604.
Tost H, Champagne FA, Meyer-Lindenberg A (2015). Environmental influence in the brain, human welfare and mental health. Nature Neuroscience, 18(10), 1421-31.
Trojano L, Grossi D, Linden DEJ, Formisano E, Hacker H, Zanella F, et al (2000). Matching two imagined clocks; the functional anatomy of spatial analysis in the absence of visual stimulation. Cerebral Cortex, (10), 473-481.
van Os J, Kenis G, Rutten BPF (2010). The environment and schizophrenia. Nature, 468(7321), 203-212.
Wilson CRE, Gaffan D, Browning PGF, Baxter MG (2010). Functional localization within the prefrontal cortex: Missing the forest for the trees? Trends in Neurosciences, 33(12), 533-540.
Zammit S, Lewis G, Rasbash J, Dalman C, Gustafsson J-E, Allebeck P (2010). Individuals, schools, and neighborhood: A multilevel longitudinal study of variation in incidence of psychotic disorders. Archives of General Psychiatry, 67(9), 914-922.
Zubin J, Spring B (1977). Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology, 86(2), 103-126.
Bargh JA, Dijksterhuis A (2001). The perception-behavior expressway: Automatic effects of social perception on social behavior. Advances in experimental social psychology (33), 1-40.
Baumeister RF, Sommer KL (1997). Consciousness, free choice, and automaticity. New Jersey: Lawrence Erlbaum Associates Publishers.
de Leon J, Verghese C, Tracy JI, Josiassen RC, Simpson GM (1994). Polydipsia and water intoxication in psychiatric patients: A review of the epidemiological literature. Biological Psychiatry, 35(6), 408-19.
Cui X, Pelekanos M, Liu PY, Burne TH, McGrath JJ, Eyles DW (2013). The vitamin d receptor in dopamine neurons; its presence in human substantia nigra and its ontogenesis in rat midbrain. Neuroscience, 16(236), 77-87.
Eyles DW, Feron F, Cui X, Kesby JP, Harms LH, Ko P, et al (2009). Developmental vitamin d deficiency causes abnormal brain development. Psychoneuroendocrinology, 34(2), 47-57.
Faris REL, Dunham HW (1939). Mental disorders in urban areas: An ecological study of schizophrenia and other psychoses. Oxford, UK: University of Chicago Press.
Flensmark J (2004). Is there an association between the use of heeled footwear and schizophrenia? Medical Hypotheses, 63(4), 740-7.
Freeman HL, Alpert M (1986). Prevalence of schizophrenia in urban population. The British Journal of Psychiatry, (149), 603-611.
Freeman D, Freeman J (2008). Paranoia the 21st century fear. Oxford, New York: Oxford University Press.
Ginovart N, Kapur S. Dopamine receptors and the treatment of schizophrenia (2010). In: Neve KA, (ed.) The dopamine receptors. New York: Springer, Humana Press, 431-77.
Golembiewski J (2012). All common psychotic symptoms can be explained by the theory of ecological perception. Medical Hypotheses, (78), 7-10.
Golembiewski J (2013). The subcortical confinement hypothesis for schizotypal hallucinations. Curēus, 5(5), 118.
Golembiewski J (2013). Are diverse factors proxies for architectural influences? A case for architecture in the aetiology of schizophrenia. Curēus, 5(3), 106.
Golembiewski J (2016). The designed environment and how it affects brain morphology and mental health. HERD, 9(2), 161-71.
Haddad L, Schafer A, Streit F, Lederbogen F, Grimm O, Wust S, et al (2014). Brain structure correlates of urban upbringing, an environmental risk factor for schizophrenia. Schizophrenia Bulletin.
Haselgrove M, Le Pelley ME, Singh NK, Teow HQ, Morris RW, Green MJ, et al (2016). Disrupted attentional learning in high schizotypy: Evidence of aberrant salience. British Journal of Psychology, 107(4), 601-24.
Kapur S (2003). Psychosis as a state of aberrant salience: A framework linking biology, phenomenology, and pharmacology in schizophrenia. American Journal of Psychiatry, 160(1), 13-23.
Kellett JM (1973). Evolutionary theory for the dichotomy of the functional psychoses. The Lancet. 301(7808), 860-863.
Kelly BD, O'Callaghan E, Waddington JL, Feeney L, Browne S, Scully PJ, et al (2010). Schizophrenia and the city: A review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophrenia Research, 116(1), 75-89.
Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J (2012). Incidence of schizophrenia and other psychoses in england, 1950–2009: A systematic review and meta-analyses. PLOS One, 7(3).
Lederbogen F, Kirsch P, Haddad L, Streit F, Tost H, Schuch P, et al (2011). City living and urban upbringing affect neural social stress processing in humans. Nature, 474(7352), 498-501.
Lederbogen F, Haddad L, Meyer-Lindenberg A (2013). Urban social stress–risk factor for mental disorders. The case of schizophrenia. Environmental Pollution, (183), 2-6.
Lhermitte F (1986). Human autonomy and the frontal lobes. Part II: Patient behavior in complex and social situations: The 'environmental dependency syndrome'. Annals of Neurology, 19(4), 335-43.
Lhermitte F, Pillon B, Serdaru M (1986). Human autonomy and the frontal lobes. Part i: Imitation and utilization behavior: A neuropsychological study of 75 patients. Annals of Neurology, 19(4), 326-34.
McGrath JA, Avramopoulos D, Lasseter VK, Wolyniec PS, Fallin MD, Liang K-Y, et al (2009). Familiality of novel factorial dimensions of schizophrenia. Archives of General Psychiatry, 66(6), 591-600.
Morgan V (2010). Physical environmental risk factors - urban environment. Sydney: Schizophrenia Research Library.
Mujica-Parodi LR, Malaspina D, Sackeim HA (2000). Logical processing, affect, and delusional thought in schizophrenia. Harvard Review of Psychiatry, 8(2), 73-83.
Rigoli F, Friston KJ, Dolan RJ (2016). Neural processes mediating contextual influences on human choice behaviour. Nature Communications, 7(12416).
Schneider SD, Jelinek L, Lincoln TM, Moritz S (2011). What happened to the voices? A fine-grained analysis of how hallucinations and delusions change under psychiatric treatment. Psychiatry Research, 188(1), 13-7.
Selten JP, Cantor-Graae E (2007). Hypothesis: Social defeat is a risk factor for schizophrenia? The British Journal of Psychiatry, 191(51), 9-12.
Stephan KE (2016). Bayesian inference, dysconnectivity and neuromodulation in schizophrenia. Brain, 139:(187), 4-6.
Torrey EF, Bowler A (1990). Geographical distribution of insanity in america: Evidence for an urban factor. Schizophrenia Bulletin, 16(4), 591-604.
Tost H, Champagne FA, Meyer-Lindenberg A (2015). Environmental influence in the brain, human welfare and mental health. Nature Neuroscience, 18(10), 1421-31.
Trojano L, Grossi D, Linden DEJ, Formisano E, Hacker H, Zanella F, et al (2000). Matching two imagined clocks; the functional anatomy of spatial analysis in the absence of visual stimulation. Cerebral Cortex, (10), 473-481.
van Os J, Kenis G, Rutten BPF (2010). The environment and schizophrenia. Nature, 468(7321), 203-212.
Wilson CRE, Gaffan D, Browning PGF, Baxter MG (2010). Functional localization within the prefrontal cortex: Missing the forest for the trees? Trends in Neurosciences, 33(12), 533-540.
Zammit S, Lewis G, Rasbash J, Dalman C, Gustafsson J-E, Allebeck P (2010). Individuals, schools, and neighborhood: A multilevel longitudinal study of variation in incidence of psychotic disorders. Archives of General Psychiatry, 67(9), 914-922.
Zubin J, Spring B (1977). Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology, 86(2), 103-126.
About the author
|
Jan Golembiewski is one of the world's leading researchers in architectural design psychology. His research traces phenomenological experience back to the neurological mechanisms that cause them. Jan is at the centre of current thinking about design for health and wellbeing. He is on the editorial board of three academic journals and has guest edited a special edition on ‘Designing the Psychiatric Milieu’. In addition, Jan regularly judges the International Academy Awards for Design and Health, and has won 18 awards for his publications, conference presentations and his teaching. Furthermore, Jan was the research lead on an international architectural health design competition, winning first prize ($1M). He is a registered architect, has served as Adjunct Professor in the Faculty of Creative Industries at QUT, Brisbane, and is a Fellow at the Centre for Urban Design and Mental Health.
|